Health Topics
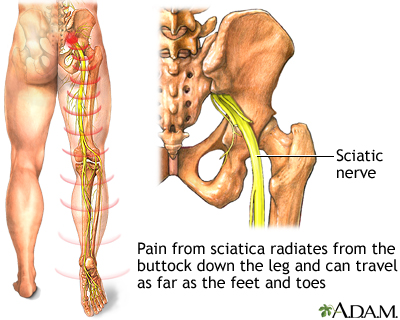
Sciatica refers to pain, weakness, numbness, or tingling in the leg. It is caused by injury to or pressure on the sciatic nerve. Sciatica is a symptom of a medical problem. It is not a medical condition by itself.
Causes
Sciatica occurs when there is pressure on or damage to the sciatic nerve. This nerve starts in the lower back and runs down the back of each leg. This nerve regulates the muscles of the back of the knee and lower leg. It also provides sensation to the back of the thigh, the outer and back part of the lower leg, and the sole of the foot.
Common causes of sciatica include:
- Slipped or herniated disk
- Spinal stenosis
- Piriformis syndrome (a pain disorder involving the narrow muscle in the buttocks)
- Pelvic injury or fracture
- Tumors
- Spondylolisthesis
Men age 30 and 50 years are more likely to have sciatica.
Symptoms
Sciatica pain can vary widely. It may feel like a mild tingling, dull ache, or burning sensation. In some cases, the pain is severe enough to make a person unable to move.
The pain most often occurs on one side of the body. Some people have sharp pain in one part of the leg or hip and numbness in other parts. The pain or numbness may also be felt on the back of the calf or on the sole of the foot. The affected leg may feel weak. Sometimes, your foot gets caught on the ground when walking.
The pain may start slowly. It may get worse:
- After standing or sitting
- During certain times of the day, such as at night
- When sneezing, coughing, or laughing, especially if caused by a herniated disk
- When bending backward or walking more than a few yards or meters, especially if caused by spinal stenosis
- When straining or holding your breath, such as during a bowel movement
Exams and Tests
Your health care provider will perform a physical exam. This may show:
- Weakness when bending the knee
- Difficulty bending the foot inward or down
- Difficulty walking on your toes
- Difficulty bending forward or backward
- Abnormal or weak reflexes
- Loss of sensation or numbness
- Pain when lifting the leg straight up when you're lying on the exam table
Tests are often not needed unless pain is severe or long-lasting. If tests are ordered, they may include:
Treatment
As sciatica is a symptom of a more specific medical condition, the underlying cause should be identified and treated.
In most cases, no surgical treatment is required and recovery occurs with conservative treatment.
Conservative (non-surgical) treatment is best in many cases. Your provider may recommend the following steps to reduce your symptoms:
- Take over-the-counter pain relievers such as ibuprofen (Advil, Motrin IB) or acetaminophen (Tylenol).
- Apply heat or ice to the painful area. Try ice for the first 48 to 72 hours, then use heat.
Measures to take care of your back at home may include:
- Bed rest is not recommended.
- Back exercises are recommended early on to strengthen your back.
- Start exercising again after 2 to 3 weeks. Include exercises to strengthen your abdominal (core) muscles and improve the flexibility of your spine.
- Reduce your activity for the first couple of days. Then, slowly start your usual activities.
- Do not do heavy lifting or twisting of your back for the first 6 weeks after the pain begins.
Your provider may also suggest physical therapy to help you learn an exercise program. Additional treatments depend on the condition that is causing the sciatica.
If these measures do not help, your provider may recommend injections of certain medicines to reduce swelling around the nerve. Other medicines may be prescribed to help reduce the stabbing pains due to nerve irritation.
Nerve pain may be very difficult to treat. If you have ongoing problems with pain, you may want to see a physiatrist (specialist in rehabilitation) or a pain specialist to ensure that you have access to the widest range of treatment options.
Surgery can be performed to relieve the compression of your spinal nerves, however, it is usually the last resort for treatment.
Outlook (Prognosis)
Often, sciatica gets better on its own. But it is common for it to return.
Possible Complications
More serious complications depend on the cause of sciatica, such as slipped disk or spinal stenosis. Sciatica can lead to permanent numbness or weakness of your leg.
When to Contact a Medical Professional
Contact your provider right away if you have:
- Unexplained fever with back pain
- Back pain after a severe blow or fall
- Redness or swelling on the back or spine
- Pain traveling down your legs below the knee
- Weakness or numbness in your buttocks, thigh, leg, or pelvis
- Burning with urination or blood in your urine
- Pain that is worse when you lie down, or awakens you at night
- Severe pain and you cannot get comfortable
- Loss of control of urine or stool (incontinence)
Also contact your provider if:
- You have been losing weight unintentionally (not on purpose)
- You use steroids or inject illicit drugs
- You have had back pain before, but this episode is different and feels worse
- This episode of back pain has lasted longer than 4 weeks
Prevention
Prevention varies, depending on the cause of the nerve damage. Avoid prolonged sitting or lying with pressure on the buttocks.
Having strong back and abdominal muscles is important to avoid sciatica. As you get older, it's a good idea to do exercises to strengthen your core.
Alternative Names
Neuropathy - sciatic nerve; Sciatic nerve dysfunction; Low back pain - sciatica; LBP - sciatica; Lumbar radiculopathy - sciatica
Patient Instructions
References
Ibrahim M, Hurlbert RJ. Nonsurgical and postsurgical management of low back pain. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 312.
Marques DR, Carroll WE. Neurology. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 41.
Review Date 8/27/2024
Updated by: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






