Health Topics

The basics of blood clots: What you need to know
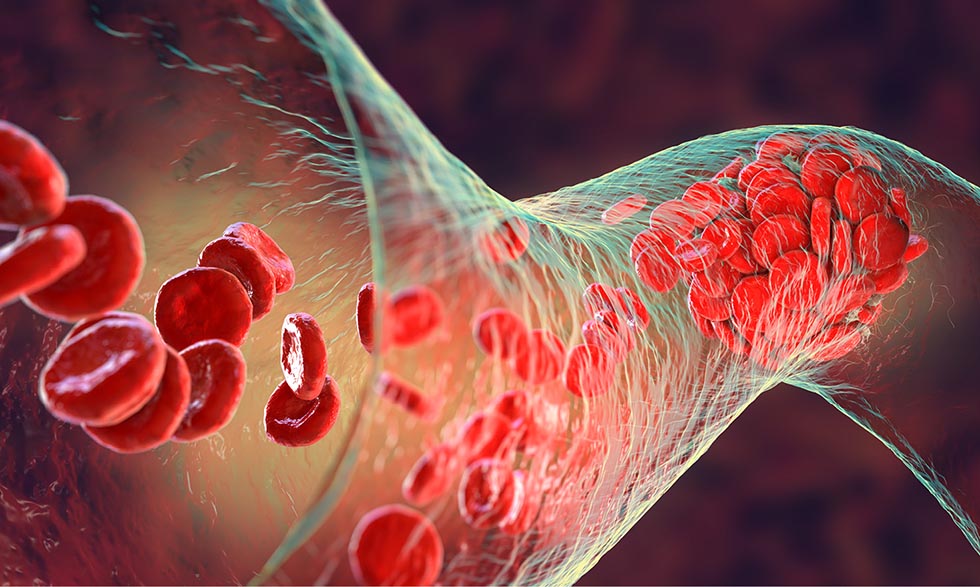
Blood clots are a natural and necessary part of healing, but they can sometimes cause serious problems.
What are blood clots?
Blood clots are made of proteins, platelets, and other cells in the blood that thicken and stick together. When you cut yourself, a blood clot forms over the injury. This stops the bleeding and helps the wound to heal. Once the injury heals, your body usually dissolves the clot.
Blood clots can also form inside the body when blood vessels are injured or damaged. These clots can block blood flow to important organs like the heart, brain, and lungs, which can cause serious health problems.
Watch this video from MedlinePlus to learn more about how blood clots form.
When blood clots go awry
Blood clots can form in your body’s blood vessels, which are part of your body’s circulatory system.
Clots that develop deep in our blood vessels can break off and travel to other parts of the body. While these clots can form anywhere in the body, they most commonly occur in the arms and legs.
Deep vein thrombosis is a blood clot that forms in a vein deep in the body. It can break loose and cause a serious problem in the lungs, called a pulmonary embolism.
Pulmonary embolism is a clot within the lungs that blocks blood flow to areas of the lung, sometimes making it difficult to breathe. Pulmonary embolism is a very dangerous condition. It can damage the lungs and other organs in the body and even cause death.
Learn more about symptoms, causes, and treatments for deep vein thrombosis and pulmonary embolism.
What causes them?
Blood clots may form when:
- There is damage to the lining of blood vessels. The damage may be caused by an acute injury, surgery and other medical procedures, or other health conditions that cause chronic inflammation.
- Blood flow is sluggish or slow. Lack of motion can cause sluggish or slow blood flow. This may occur after surgery, if you’re ill and in bed for a long time, or during extended travel.
- Your blood is thicker or more likely to clot than normal. Certain conditions can increase blood’s tendency to clot. So can some medical treatments such as chemotherapy (which treats cancer) or birth control pills.
Often, blood clots form without any clear cause.
What are some common symptoms?
Blood clot symptoms will vary based on where the clot is located. Many symptoms of blood clots are the same as symptoms of other conditions. You can also have a clot and not experience any noticeable symptoms.
In an arm or leg. If you have a clot in your arms or legs, it could be a deep vein thrombosis. You might experience:
- Pain (either sudden or gradual)
- Swelling
- Tenderness (hurts when touched)
- Warmth or redness
In the lungs. A clot in the lungs (pulmonary embolism) can cause symptoms such as:
- Shortness of breath
- Chest pain (especially with deep breathing)
- Sweating or a fever
- Coughing up blood
In the abdomen. Blood clots can also form in the blood vessels inside the abdomen. They can cause severe abdominal pain and digestive issues (such as nausea and vomiting).
The only way to find out whether you have a blood clot is to get medical help. If you know the warning signs, you’re more likely to recognize them and get help as soon as possible.
Who is at risk?
Blood clots can affect anyone, but some factors can increase your risk. They include:
- Age. Clots can occur at any age, but people older than 60 are at greatest risk.
- Family history. If your family has a history of clots or clotting disorders, you are more likely to develop them.
- Lack of movement. Sitting or lying down for a long time (for example, during a long flight or extended hospital stay) reduces blood flow, which increases your risk of clots.
- Pregnancy and childbirth. Blood is more likely to clot during pregnancy, making pregnant people more susceptible. This risk can last through the first six weeks after the baby is born.
- Certain health conditions. These include cancer (and cancer treatment), heart disease, diabetes, blood disorders, certain autoimmune conditions, and COVID-19.
- Certain medications. Some medications can slow blood flow and cause clotting. These include drugs that affect the hormone estrogen (such as birth control pills).
- Smoking. Smoking damages blood vessels and makes it more difficult for blood to clot properly.
If you have multiple risk factors, you’re more likely to develop blood clots.
How are blood clots diagnosed?
If your health care provider suspects that you may have a blood clot, they will ask you about your symptoms and medical history and perform a physical exam.
To learn about your medical history, they may ask about:
- Your overall health
- Any prescription medicines you’re taking
- Any recent surgeries or injuries you’ve had
- Whether you’ve been treated for cancer
During the physical exam, they will:
- Check for signs of blood clots
- Check your blood pressure, your heart, and your lungs
They may also order tests such as a blood test or an imaging test to diagnose a clot or a clotting disorder. These can include:
- Ultrasound. This is the most common test for diagnosing blood clots in the arms and legs. Ultrasound uses sound waves to create pictures of blood flowing through the arteries and veins.
- D-dimer test. This blood test measures a substance in the blood that’s released when a blood clot dissolves. If the test shows high levels of this substance, you may have a clotting disorder.
- Other tests. If the doctor suspects a clot in the lungs, they may order additional imaging tests to confirm the diagnosis. These tests provide detailed images of the lungs and can help pinpoint the location of a blood clot.
How are they treated?
Blood thinners are the most common treatment for blood clots. These medications help prevent new clots from forming and keep existing clots from getting bigger. However, they can’t break up clots that have already formed.
In some cases, doctors may use clot-dissolving medications to break up clots that have already formed. Very rarely, surgery may be necessary to remove a blood clot. These treatments are less common and depend on the type of clot, its severity, and where it’s located.
If you have a blood clot, it is important to work with your doctor to develop a treatment plan that is right for you.
How to prevent blood clots
Here are some steps you can take to lower your chances of developing blood clots.
- Stay active. Exercise keeps your blood flowing, which makes it harder for clots to develop.
- Take movement breaks. It’s important to move your body regularly, especially during long trips or extended periods of sitting. If you can, get up and move around every 2 to 3 hours.
- Stay hydrated. Drink plenty of fluid to keep your blood flowing.
- Say no to smoking. Kicking the habit is a win-win for your overall health. And if you don’t smoke, don’t start!
- Maintain a healthy weight. Excess body weight can increase your risk of blood clots. If you're concerned about how your weight might affect your risk for blood clots, talk to your doctor about safe and effective weight management strategies.
- Follow the doctor’s orders. If your doctor prescribes blood thinners, follow their instructions closely.
- Try compression stockings. Your doctor may recommend these to improve blood flow in your legs and arms.