Health Topics
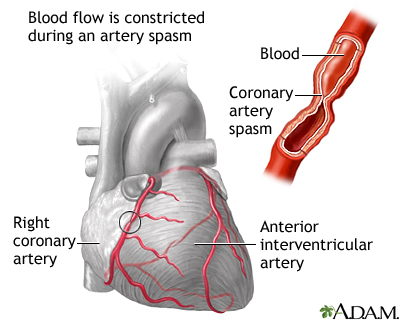
The coronary arteries supply blood and oxygen to the heart. Coronary artery spasm is a brief, sudden narrowing of one of these arteries.
Causes
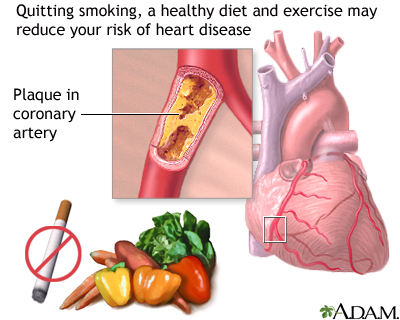
Coronary artery spasm often occurs in coronary arteries that have not become hardened due to plaque buildup. However, it also can occur in arteries with plaque buildup.
These spasms are due to a squeezing of muscles in the artery wall. They most often occur in just one area of the artery. The coronary artery may appear normal during testing, but it does not function normally at other times.
About 2% of people with angina (chest pain and pressure) have coronary artery spasm.

Coronary artery spasm occurs most commonly in people who smoke or who have high cholesterol or high blood pressure. It may occur without cause, or it may be triggered by:
- Alcohol withdrawal
- Emotional stress
- Exposure to cold
- Medicines that cause narrowing of the blood vessels (vasoconstriction)
- Stimulant drugs, such as amphetamines and cocaine
Cocaine use and cigarette smoking can cause severe spasms of the arteries. This causes the heart to work harder. In many people, coronary artery spasm may occur without any other heart risk factors (such as smoking, diabetes, high blood pressure, and high cholesterol).
Symptoms
Spasm may be "silent" (without symptoms) or it may result in chest pain or angina. If the spasm lasts long enough, it may even cause a heart attack.
The main symptom is a type of chest pain called angina. Typically, the chest pain feels like tightness, heavy pressure, squeezing, or a crushing feeling. It may spread to the:
- Arm (most often the left)
- Back
- Jaw
- Neck
- Shoulder
Some people say the pain feels like gas or indigestion. It is most often severe. The pain may spread to the neck, jaw, shoulder, or arm.
The pain of coronary artery spasm:
- Often occurs at rest
- May occur at the same time each day, usually between midnight and 8:00 a.m.
- Lasts from 5 to 30 minutes
The person may lose consciousness.
Chest pain and shortness of breath due to coronary artery spasm are often not caused by exercise, unlike angina that is caused by hardening of the coronary arteries.
Exams and Tests
Tests to diagnose coronary artery spasm may include:
- Coronary angiography
- Electrocardiogram (ECG)
- Echocardiography
Treatment
The goal of treatment is to control chest pain and prevent a heart attack. A medicine called nitroglycerin (NTG) can relieve an episode of pain.
Your health care provider may prescribe other medicines to prevent chest pain. You may need long term treatment with a type of medicine called a calcium channel blocker or a long-acting nitrate.
Beta-blockers are another type of medicine that is used with other coronary artery problems. However, beta-blockers may make coronary artery spasm worse. They should be used with care.
If you have this condition, you should avoid coronary artery spasm triggers. These include exposure to cold, cocaine or amphetamine use, cigarette smoking, and high-stress situations.
Outlook (Prognosis)
Coronary artery spasm is a long-term (chronic) condition. However, treatment most often helps control symptoms.
The disorder may be a sign that you have a high risk for heart attack or deadly irregular heart rhythms. The outlook is most often good if you follow your treatment, your provider's advice, and avoid certain triggers.
Possible Complications
Complications may include:
- Abnormal heart rhythms, which may cause cardiac arrest and sudden death
- Heart attacks
When to Contact a Medical Professional
Immediately call the local emergency number (such as 911) or go to the hospital emergency room if you have a history of angina and the crushing or squeezing chest pain is not relieved by nitroglycerin. The pain may be due to a heart attack. Rest and nitroglycerin often do not completely relieve the pain of a heart attack.
A heart attack is a medical emergency. If you have symptoms of a heart attack, seek medical help right away.
Prevention
Take steps to reduce your risk of developing heart disease. Some studies have shown that making a few lifestyle changes can reduce your risk for heart disease. Lifestyle changes can also help prevent some angina attacks. Your provider may tell you to:
- Lose weight if you are overweight
- Stop smoking
- Exercise regularly
- Drink alcohol in moderation only
- Eat a healthy diet that is high in vegetables, fruits, whole grains, fish, and lean meats
Alternative Names
Variant angina; Angina - variant; Prinzmetal angina; Vasospastic angina; Chest pain - Prinzmetal
Patient Instructions
References
Boden WE. Angina pectoris and chronic ischemic heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 56.
Bonaca MP, Sabatine MS. Approach to the patient with chest pain. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 35.
Giugliano RP, Braunwald E. Non-ST elevation acute coronary syndromes. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 39.
Lange RA, Mukherjee D. Acute coronary syndrome: unstable angina and non-ST elevation myocardial infarction. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 57.
Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187-e285. PMID: 34756653 pubmed.ncbi.nlm.nih.gov/34756653/.
Review Date 1/1/2025
Updated by: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.







