Health Topics
Mitral regurgitation is a disorder in which the mitral valve on the left side of the heart does not close properly.
Regurgitation means leaking from a valve that does not close all the way.
Causes
Blood that flows between different chambers of your heart must flow through a valve. The valve between the 2 chambers on the left side of your heart is called the mitral valve. It opens up enough so that blood can flow from the upper chamber of your heart (left atrium) to the lower chamber (left ventricle). It then closes, keeping blood from flowing backwards.
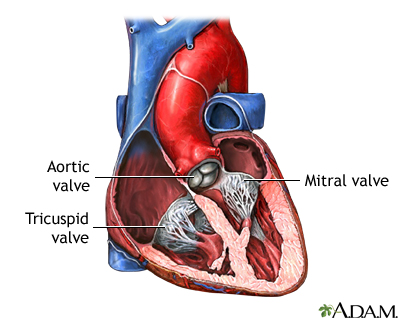
When the mitral valve doesn't close all the way, blood flows backward into the upper heart chamber (atrium) from the lower chamber as it contracts. This is called mitral regurgitation and is a common type of heart valve disorder. This cuts down on the amount of blood that flows to the rest of the body. As a result, the heart may try to pump harder. This may lead to congestive heart failure.
Mitral regurgitation may begin suddenly. This often occurs after a heart attack. When the regurgitation does not go away, it becomes long-term (chronic).
Many other diseases or problems can weaken or damage the valve or the heart tissue around the valve. You are at risk for mitral valve regurgitation if you have:
- Coronary heart disease and high blood pressure
- Infection of the heart valves
- Mitral valve prolapse (MVP)
- Rare conditions, such as untreated syphilis or Marfan syndrome
- Rheumatic heart disease. This is a complication of untreated strep throat that is becoming less common.
- Swelling of the left lower heart chamber
Another important risk factor for mitral regurgitation is past use of a diet pill called "Fen-Phen" (fenfluramine and phentermine) or dexfenfluramine. The drug was removed from the market by the U.S. Food and Drug Administration (FDA) in 1997 because of safety concerns.
Symptoms
Symptoms may begin suddenly if:
- A heart attack damages the muscles around the mitral valve.
- The cords that attach the muscle to the valve break.
- An infection of the valve destroys part of the valve.
There are often no symptoms. When symptoms occur, they often develop gradually, and may include:
- Cough
- Fatigue, exhaustion, and lightheadedness
- Rapid breathing
- Sensation of feeling the heart beat (palpitations) or a rapid heartbeat
- Shortness of breath that increases with activity and when lying down
- Waking up an hour or so after falling asleep because of trouble breathing
- Urination, excessive at night
Exams and Tests
When listening to your heart and lungs, the health care provider may detect:
- A thrill (vibration) over the heart when feeling the chest area
- An extra heart sound (S4 gallop)
- A distinctive heart murmur
- Crackles in the lungs (if fluid backs up into the lungs)
The physical exam may also reveal:
- Ankle and leg swelling
- Enlarged liver
- Bulging neck veins
- Other signs of right-sided heart failure
The following tests may be done to look at the heart valve structure and function:
- CT scan of the heart
- Echocardiogram (an ultrasound examination of the heart) - transthoracic or transesophageal
- Magnetic resonance imaging (MRI)
Cardiac catheterization may be done if heart function becomes worse.
Treatment
Treatment will depend on what symptoms you have, what condition caused the mitral valve regurgitation, how well the heart is working, and if the heart has become enlarged.
People with high blood pressure or a weakened heart muscle may be given medicines to reduce the strain on the heart and ease symptoms.
The following medicines may be prescribed when mitral regurgitation symptoms get worse:
- Beta-blockers, ACE inhibitors, or calcium channel blockers
- Blood thinners (anticoagulants) to help prevent blood clots in people with atrial fibrillation
- Medicines that help control uneven or abnormal heartbeats
- Water pills (diuretics) to remove excess fluid in the lungs
A low-sodium diet may be helpful. You may need to limit your activity if symptoms develop.
Once the diagnosis is made, you should visit your provider regularly to track your symptoms and heart function.
You may need surgery to repair or replace the valve if:
- Heart function is poor
- The heart becomes enlarged (dilated)
- Symptoms get worse
Catheter based non-surgical techniques to place clips or replace the mitral valve are increasingly in use for some selected patients with mitral regurgitation.
Outlook (Prognosis)
The outcome varies. Most of the time the condition is mild, so no therapy or restriction is needed. Symptoms can most often be controlled with medicine.
Possible Complications
Problems that may develop include:
- Abnormal heart rhythms, including atrial fibrillation and possibly more serious, or even life-threatening abnormal rhythms
- Clots that may travel to other areas of the body, such as the lungs or brain
- Infection of the heart valve
- Heart failure
When to Contact a Medical Professional
Contact your provider if symptoms get worse or do not improve with treatment.
Also contact your provider if you are being treated for this condition and develop signs of infection, which include:
- Chills
- Fever
- General ill feeling
- Headache
- Muscle aches
Prevention
People with abnormal or damaged heart valves are at risk for an infection called endocarditis. Anything that causes bacteria to get into your bloodstream can lead to this infection. Steps to avoid this problem include:
- Avoid unclean injections.
- Treat strep infections quickly to prevent rheumatic fever.
- Always tell your provider and dentist if you have a history of heart valve disease or congenital heart disease before treatment. Some people may need antibiotics before dental procedures or surgery.
Alternative Names
Mitral valve regurgitation; Mitral valve insufficiency; Heart mitral regurgitation; Valvular mitral regurgitation
References
Carabello BA, Kodali S. Valvular heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 60.
Hahn RT, Bonow RO. Mitral regurgitation. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 76.
Writing Committee Members, Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2021;162(2):e183-e353. PMID: 33972115 pubmed.ncbi.nlm.nih.gov/33972115/.
Review Date 2/27/2024
Updated by: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.





