Health Topics
Hysterectomy is surgery to remove a woman's womb (uterus). The uterus is a hollow muscular organ that nourishes the developing baby during pregnancy.
Description
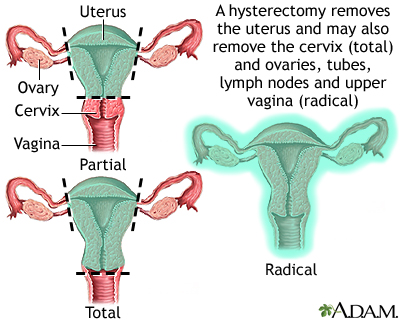
You may have all or part of the uterus removed during a hysterectomy. The fallopian tubes and ovaries may also be removed.
There are many different ways to perform a hysterectomy. It may be done through:
- A surgical cut in the belly (called an open or abdominal hysterectomy)
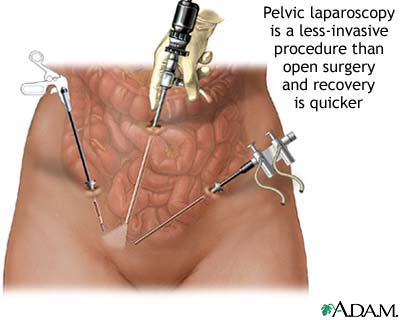
- Three to four small surgical cuts in the belly and then using a laparoscope
- A surgical cut in the vagina, aided by the use of a laparoscope (called a vaginal hysterectomy)
- A surgical cut in the vagina without the use of a laparoscope (called a vaginal hysterectomy)
- Three to four small surgical cuts in the belly, in order to perform robotic surgery
You and your surgeon will decide which type of procedure. The choice will depend on your medical history and the reason for the surgery.
Why the Procedure is Performed
There are many reasons a woman may need a hysterectomy, including:
- Adenomyosis, a condition that causes heavy, painful periods
- Cancer of the uterus, most often endometrial cancer
- Cancer of the cervix or changes in the cervix called cervical dysplasia that may lead to cancer
- Cancer of the ovary
- Long-term (chronic) pelvic pain
- Severe endometriosis that does not get better with other treatments
- Severe, long-term vaginal bleeding that is not controlled with other treatments
- Slipping of the uterus into the vagina (uterine prolapse)
- Tumors in the uterus, such as uterine fibroids
- Uncontrolled bleeding during childbirth
- Severe infection involving the uterus (for example, pelvic inflammatory disease)
Hysterectomy is a major surgery. Some conditions can be treated with medicines or less invasive procedures such as:
- Uterine artery embolization
- Endometrial ablation
- Using birth control pills
- Using pain medicines
- Using an IUD (intrauterine device) that releases the hormone progestin
- Pelvic laparoscopy
Risks
Risks of any surgery are:
- Allergic reactions to medicines
- Breathing problems
- Blood clots, which may cause death if they travel to the lungs
- Bleeding
- Infection
- Injury to nearby body areas
Risks of a hysterectomy are:
- Injury to the bladder or ureters
- Pain during sexual intercourse
- Early menopause if the ovaries are removed
- Decreased interest in sex
- Increased risk of heart disease if the ovaries are removed before menopause
Before the Procedure
Before deciding to have a hysterectomy, ask your health care provider what to expect after the procedure. Many women notice changes in their body and in how they feel about themselves after a hysterectomy. Talk with your provider, family, and friends about these possible changes before you have surgery.
Tell your health care team about all the medicines you are taking. These include herbs, supplements, and other medicines you bought without a prescription.
During the days before the surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), clopidogrel (Plavix), warfarin (Coumadin), and any other medicines like these.
- Ask your surgeon which medicines you should still take on the day of your surgery.
- If you smoke, try to stop. Ask your provider for help quitting.
On the day of your surgery:
- You will most often be asked not to drink or eat anything for 8 hours before the surgery.
- Take any medicines your provider told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
After surgery, you will be given pain medicines.
You may also have a tube, called a catheter, inserted into your bladder to pass urine. Most of the time, the catheter is removed before leaving the hospital.
You will be asked to get up and move around as soon as possible after surgery. This helps prevent blood clots from forming in your legs and speeds recovery.
You will be asked to get up to use the bathroom as soon as you are able. You may return to a normal diet as soon as you can without causing nausea and vomiting.
How long you stay in the hospital depends on the type of hysterectomy.
- You can likely go home the next day when surgery is done through the vagina, with a laparoscope, or after robotic surgery.
- When a larger surgical cut (incision) in the abdomen is made, you may need to stay in the hospital for 1 to 2 days. You may need to stay longer if the hysterectomy is done because of cancer.
Outlook (Prognosis)
How long it takes you to recover depends on the type of hysterectomy. Average recovery times are:
- Abdominal hysterectomy: 4 to 6 weeks
- Vaginal hysterectomy: 3 to 4 weeks
- Robot-assisted or total laparoscopic hysterectomy: 2 to 4 weeks
A hysterectomy will cause menopause if you also have your ovaries removed. Removal of the ovaries can also lead to a decreased sex drive. Your doctor may recommend estrogen replacement therapy. Discuss with your provider the risks and benefits of this therapy.
If the hysterectomy was done for cancer, you may need further treatment.
Alternative Names
Vaginal hysterectomy; Abdominal hysterectomy; Supracervical hysterectomy; Radical hysterectomy; Removal of the uterus; Laparoscopic hysterectomy; Laparoscopically assisted vaginal hysterectomy; LAVH; Total laparoscopic hysterectomy; TLH; Laparoscopic supracervical hysterectomy; Robotically assisted hysterectomy
References
Committee on Gynecologic Practice. Committee opinion no 701: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2017;129(6):e155-e159. PMID: 28538495 pubmed.ncbi.nlm.nih.gov/28538495/.
Karram MM. Vaginal hysterectomy. In: Baggish MS, Karram MM, eds. Atlas of Pelvic Anatomy and Gynecologic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 51.
Prescott LS, Yunker AC, Alvarez R. Gynecologic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 71.
Thakar R. Is the uterus a sexual organ? Sexual function following hysterectomy. Sex Med Rev. 2015;3(4):264-278. PMID: 27784599 pubmed.ncbi.nlm.nih.gov/27784599/.
Review Date 3/31/2024
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.







