Health Topics
Low back pain refers to pain that you feel in your lower back. You may also have back stiffness, decreased movement of the lower back, and difficulty standing straight.
Acute back pain can last for a few days to a few weeks.
Causes
Most people have at least one backache in their life. Although this pain or discomfort can happen anywhere in your back, the most common area affected is your lower back. This is because the lower back supports most of your body's weight.
Low back pain is the number two reason that Americans see their health care provider. It is second only to colds and flu.
You will usually first feel back pain just after you lift a heavy object, move suddenly, sit in one position for a long time, or have an injury or accident.
Acute low back pain is most often caused by a sudden injury to the muscles and ligaments supporting the back. The pain may be caused by muscle spasms or a strain or tear in the muscles and ligaments.
Causes of sudden low back pain include:
- Compression fractures of the spine (often due to osteoporosis)
- Cancer involving the spine
- Fracture of a spine bone
- Muscle spasm (very tense muscles)
- Ruptured or herniated disk
- Sciatica
- Spinal stenosis (narrowing of the spinal canal)
- Spine curvatures (like scoliosis or kyphosis), which may be inherited and seen in children or teens
- Strain or tears to the muscles or ligaments supporting the back
Low back pain may also be due to:
- An abdominal aortic aneurysm that is leaking
- Arthritis conditions, such as osteoarthritis, psoriatic arthritis, and rheumatoid arthritis
- Infection of the spine (osteomyelitis, diskitis, abscess)
- Kidney infection or kidney stones
- Problems related to pregnancy
- Problems with your gall bladder or pancreas
- Medical conditions that affect the female reproductive organs, including endometriosis, ovarian cysts, ovarian cancer, or uterine fibroids
- Pain around the back of your pelvis, or sacroiliac (SI) joint
Symptoms
You may feel a variety of symptoms if you have hurt your back. You may have a tingling or burning sensation, a dull achy feeling, or sharp pain. The pain may be mild, or it can be so severe that you are unable to move.
Depending on the cause of your back pain, you may also have pain in your leg, hip, or the bottom of your foot. You may also have weakness in your legs and feet.
Exams and Tests
When you first see your provider, you will be asked about your back pain, including its location, how often it happens and how severe it is.
Your provider will try to determine the cause of your back pain and whether it is likely to quickly get better with simple measures such as ice, mild painkillers, physical therapy, and proper exercises. Most of the time, back pain will get better using these methods.
During the physical exam, your provider will try to pinpoint the location of the pain and figure out how it affects your movement.
Most people with back pain improve or recover within 4 to 6 weeks and often much sooner than that. Your provider may not order any tests of your spine during the first visit or for 4 to 6 weeks unless you have certain symptoms.
Tests that might be ordered include:
- Blood tests such as a complete blood count (CBC) or erythrocyte sedimentation rate (ESR)
- X-ray
- CT scan of the lower spine
- MRI of the lower spine
Treatment
To get better quickly, take the right measures when you first feel pain.
Here are some tips for how to handle pain:
- Stop or reduce normal physical activity for the first few days. This will help relieve your symptoms and reduce any swelling in the area of the pain.
- Apply heat or ice to the painful area. One good method is to use ice for the first 48 to 72 hours and then use heat.
- Take over-the-counter pain relievers such as ibuprofen (Advil, Motrin) or acetaminophen (Tylenol). Follow package instructions on how much to take. Do not take more than the recommended amount.
While sleeping, try lying in a curled-up, fetal position with a pillow between your legs. If you usually sleep on your back, place a pillow or rolled towel under your knees to relieve pressure.
A common misbelief about back pain is that you need to rest and avoid activity for a long time. In fact, bed rest is not recommended. If you have no sign of a serious cause for your back pain (such as loss of bowel or bladder control, weakness, weight loss, or fever), then you should stay as active as possible. It is important to prevent your back and abdominal muscles from becoming too weak.
You should reduce your activity only for the first couple of days. Then, slowly start your usual activities after that. Do not perform activities that involve heavy lifting or twisting of your back for the first 6 weeks after the pain begins. After 2 to 3 weeks, you should gradually start exercising again.
- Begin with light aerobic activity. Walking, riding a stationary bicycle, and swimming are great examples. These activities can improve blood flow to your back and promote healing. They also strengthen muscles in your stomach and back.
- You may benefit from physical therapy. Your provider will determine whether you need to see a physical therapist and can refer you to one. The physical therapist will first use methods to reduce your pain. Then, the therapist will teach you ways to prevent getting back pain again.
- Stretching and strengthening exercises are important. But, starting these exercises too soon after an injury can make your pain worse. A physical therapist can tell you when to begin stretching and strengthening exercises and how to do them.
If your pain lasts longer than 1 month, your primary provider may send you to see a physiatrist (specialist in rehabilitation), or an orthopedist (bone specialist).
If your pain has not improved after use of medicines, physical therapy, and other treatments, your provider may recommend an epidural injection.
You may also see:
- A massage therapist
- Someone who performs acupuncture
- Someone who does spinal manipulation (a chiropractor, osteopathic doctor, or physical therapist)
Sometimes, a few visits to these specialists will help back pain.
Outlook (Prognosis)
Many people feel better within 1 week. After another 4 to 6 weeks, the back pain should be completely gone.
When to Contact a Medical Professional
Contact your provider right away if you have:
- Back pain after a severe blow or fall
- Burning with urination or blood in your urine
- A history of cancer
- Loss of control over urine or stool (incontinence)
- Pain traveling down your legs below the knee
- Pain that is worse when you lie down or pain that wakes you up at night
- Redness or swelling on the back or spine
- Severe pain that does not allow you to get comfortable
- Unexplained fever with back pain
- Weakness or numbness in your buttocks, thigh, leg, or pelvis
- Difficulty walking or maintaining your balance
Also contact your provider if:
- You have been losing weight unintentionally
- You use steroids or intravenous drugs
- You have had back pain before, but this episode is different and feels worse
- This episode of back pain has lasted longer than 4 weeks
Prevention
There are many things you can do to lower your chances of getting back pain. Exercise is important for preventing back pain. Through exercise you can:
- Improve your posture
- Strengthen your back and improve flexibility
- Lose weight
- Avoid falls
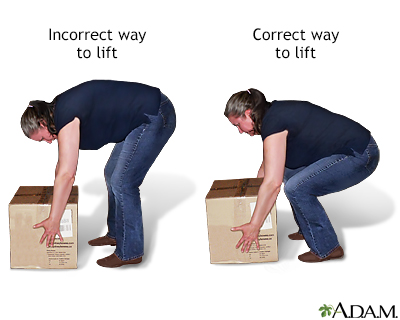
It is also very important to learn to lift and bend properly. Follow these tips:
- If an object is too heavy or awkward, get help.
- Spread your feet apart to give your body a wide base of support when lifting.
- Stand as close as possible to the object you are lifting.
- Bend at your knees, not at your waist.
- Tighten your stomach muscles as you lift the object or lower it down.
- Hold the object as close to your body as you can.
- Lift using your leg muscles.
- As you stand up with the object, do not bend forward.
- Do not twist while you are bending down for the object, lifting it up, or carrying it.
Other measures to prevent back pain include:
- Avoid standing for long periods. If you must stand for your work, alternate resting each foot on a stool.
- Do not wear high heels. Use cushioned soles when walking.
- When sitting for work, especially if you are using a computer, make sure your chair has a straight back with an adjustable seat and back, armrests, and a swivel seat.
- Use a stool under your feet while sitting so that your knees are higher than your hips.
- Place a small pillow or rolled towel behind your lower back while sitting or driving for long periods.
- If you drive a long distance, stop and walk around every hour. Bring your seat as far forward as possible to avoid bending. Do not lift heavy objects just after a ride.
- Quit smoking.
- Lose weight.
- Do exercises on a regular basis to strengthen your abdominal and core muscles. This will strengthen your core to decrease the risk for further injuries.
- Learn to relax. Try methods such as yoga, tai chi, or massage.
Alternative Names
Backache; Low back pain; Lumbar pain; Pain - back; Acute back pain; Back pain - new; Back pain - short-term; Back strain - new
Patient Instructions
References
Corwell BN, Davis NL. Back pain. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 31.
El Abd OH, Amadera JED. Low back strain or sprain. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 48.
Grabowski G, Gilbert TM, Larson EP, Cornett CA. Degenerative conditions of the cervical and thoracolumbar spine. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 130.
Malik K, Nelson A. Overview of low back pain disorders. In: Benzon HT, Raja SN, Liu SS, Fishman SM, Cohen SP, eds. Essentials of Pain Medicine. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 24.
Murray EL, Misulis KE. Lower back and lower limb pain. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 33.
Review Date 6/17/2024
Updated by: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.








