Health Topics
Polyarteritis nodosa is a serious inflammatory blood vessel disease. The small and medium-sized arteries become swollen and damaged.
Causes
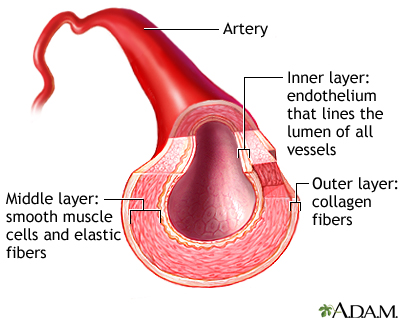
Arteries are the blood vessels that carry oxygen-rich blood to organs and tissues. The cause of polyarteritis nodosa is unknown. The condition occurs when certain immune cells attack the affected arteries. The tissues that are fed by the affected arteries do not get the oxygen and nourishment they need. Damage occurs as a result.
More adults than children get this disease.
People with active hepatitis B or hepatitis C may develop this disease.
Symptoms
Symptoms are caused by damage to affected organs. The skin, joints, muscles, gastrointestinal tract, heart, kidneys, and nervous system are often affected.
Symptoms include:
- Abdominal pain
- Decreased appetite
- Fatigue
- Fever
- Joint aches
- Muscle aches
- Unintentional weight loss
- Weakness
If nerves are affected, you may have numbness, pain, burning, and weakness. Damage to the nervous system may cause strokes or seizures.
Exams and Tests
No specific lab tests are available to diagnose polyarteritis nodosa. There are a number of disorders that have features similar to polyarteritis nodosa. These are known as "mimics."
You will have a complete physical exam.
Lab tests that can help make the diagnosis and check for disease mimics include:
- Complete blood count (CBC) with differential, creatinine, tests for hepatitis B and C, and urinalysis
- Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP)
- Serum protein electrophoresis
- Serum complement levels
- HIV test
- Hepatitis B and hepatitis C tests
- Cryoglobulins
- Anti-phospholipid antibodies
- Blood cultures
- Other blood tests will be done to check for similar conditions, such as systemic lupus erythematosus (ANA) or granulomatosis with polyangiitis (ANCA)
- Arteriogram
- Tissue biopsy
Treatment
Treatment involves medicines to suppress inflammation and the immune system. These may include steroids, such as prednisone. Similar medicines, such as azathioprine, methotrexate or mycophenolate that allow for reducing the dose of steroids are often used as well. Cyclophosphamide is used in severe cases.
For polyarteritis nodosa related to hepatitis, treatment may involve plasmapheresis and antiviral medicines.
Outlook (Prognosis)
Current treatments with steroids and other medicines that suppress the immune system (such as azathioprine or cyclophosphamide) can improve symptoms and the chance of long-term survival.
The most serious complications most often involve the kidneys and gastrointestinal tract.
Without treatment, the outlook is poor.
Possible Complications
Complications may include:
- Heart attack
- Intestinal necrosis and perforation
- Kidney failure
- Stroke
When to Contact a Medical Professional
Contact your health care provider if you develop symptoms of this disorder. Early diagnosis and treatment may improve the chance of a good outcome.
Prevention
There is no known prevention. However, early treatment can prevent some damage and symptoms.
Alternative Names
Periarteritis nodosa; PAN; Systemic necrotizing vasculitis
References
Luqmani R, Awisat A. Polyarteritis nodosa and related disorders. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 95.
Shanmugam VK. Vasculitis and other uncommon arteriopathies. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 138.
Stone JH. The systemic vasculitides. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 249.
Review Date 5/9/2024
Updated by: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






